Central Serous Chorioretinopathy (CSR)
Central Serous Chorioretinopathy (CSCR) is an eye condition that affects the retina, leading to visual disturbances. It is characterized by fluid accumulation under the central portion of the retina, called the macula. This buildup of fluid causes blurred or distorted vision, which can significantly impact daily activities such as reading, driving, or using electronic devices.
While CSCR is often self-limiting, meaning that it resolves on its own in many cases, some patients may experience persistent or recurrent episodes that require medical intervention. Understanding the causes, risk factors, natural course, and treatment options for CSCR is crucial in managing the condition effectively.
What is Central Serous Chorioretinopathy?
CSCR is an eye disease that occurs when fluid leaks from the choroid (a layer of blood vessels beneath the retina) into the retinal layers, leading to a serous detachment of the macula. The macula is responsible for central vision, and when affected, patients may experience blurred or distorted vision.
CSCR primarily affects men between the ages of 20 and 50, but it can also occur in women and older individuals. In most cases, the condition resolves within a few months, but some individuals may develop chronic or recurrent CSCR, leading to long-term visual problems.
Causes of CSCR
The exact cause of CSCR is not fully understood, but it is believed to result from increased permeability of the choroidal blood vessels. Several physiological and biochemical factors contribute to the development of CSCR, including:
- Choroidal hyperpermeability – Increased leakage of fluid from the choroid into the retina.
- Dysregulation of the retinal pigment epithelium (RPE) – The RPE normally acts as a barrier and pump to remove excess fluid. When it malfunctions, fluid accumulates under the retina.
- Autonomic dysfunction – An imbalance in the nervous system may contribute to abnormal blood vessel function, increasing the risk of fluid leakage.
Risk Factors for CSCR
Several factors can increase the likelihood of developing CSCR. Understanding these risk factors can help in modifying lifestyle habits to reduce the risk of recurrence.
1. Stress and Corticosteroid Use
Psychological stress: CSCR has been strongly associated with high-stress levels. The body’s response to stress leads to increased production of corticosteroids, which can impact choroidal blood flow and permeability.
Corticosteroid use: Systemic or topical steroids, including nasal sprays, inhalers, skin creams, and injections, can trigger or worsen CSCR by increasing fluid leakage from the choroid.
2. Hormonal Factors
Elevated levels of cortisol and epinephrine, particularly in individuals with a high-stress lifestyle, have been linked to CSCR. Some cases occur during pregnancy due to hormonal changes.
3. Hypertension and Cardiovascular Disease
High blood pressure and cardiovascular conditions can contribute to abnormal blood vessel function in the choroid, increasing susceptibility to CSCR.
4. Type A Personality
Individuals who are highly competitive, ambitious, and work in high-stress environments have been found to be more prone to developing CSCR.
5. Sleep Disturbances and Shift Work
People with irregular sleep patterns, including those who work night shifts or experience chronic sleep deprivation, may have an increased risk of developing CSCR.
6. Medications and Substance Use
Use of medications such as decongestants, erectile dysfunction drugs, and stimulants can increase the risk. Excessive alcohol and caffeine consumption have also been linked to CSCR.
7. Helicobacter Pylori Infection
Some studies suggest a possible association between H. pylori infection (a bacteria affecting the stomach) and CSCR.
8. Genetic Predisposition
There is some evidence that CSCR may have a genetic component, with a higher likelihood of occurrence in individuals with a family history of the condition.
Symptoms of CSCR
- Blurred or hazy central vision
- Distorted vision (metamorphopsia), where straight lines appear wavy
- Dark or gray spots in central vision
- Reduced contrast sensitivity
- Difficulty with night vision
- Micropsia, where objects appear smaller than they are
- Mild color vision changes
Diagnosis of CSCR
Your ophthalmologist will perform several tests to confirm CSCR, including:
1. Dilated Fundus Examination – To assess retinal changes.
2. Optical Coherence Tomography (OCT) – A non-invasive imaging test that provides cross-sectional images of the retina to detect fluid accumulation.
3. Fluorescein Angiography (FA) – Uses a dye injected into the bloodstream to visualize leaking blood vessels.
4. Indocyanine Green Angiography (ICGA) – Helps in detecting choroidal abnormalities.
Natural History of CSCR
The progression of CSCR varies from patient to patient. Most cases follow one of the three patterns:
1. Acute CSCR (Self-limiting Form)
• The most common form.
• Symptoms develop suddenly and may include blurred vision, central scotoma (dark spot in vision), and distortion (metamorphopsia).
• In 80-90% of cases, fluid resolves within 3-6 months without treatment, and vision returns to near-normal levels.
2. Chronic CSCR
• In some cases, fluid persists for more than 6 months.
• The prolonged presence of fluid leads to damage to the retinal pigment epithelium, causing permanent visual impairment.
3. Recurrent CSCR
• Some individuals experience repeated episodes of CSCR over the years.
• With each recurrence, vision may become progressively worse due to cumulative damage to the macula.
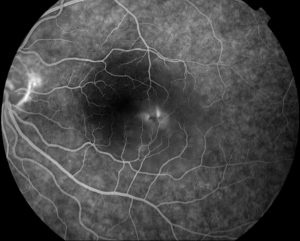
FFA showing smoke stack appearance of dye leakage in active CSCR.
Treatment Options for CSCR
Most cases of acute CSCR resolve spontaneously without treatment. However, if vision does not improve or if CSCR becomes chronic, several treatment options are available:
1. Observation (Watchful Waiting)
Recommended for patients with mild symptoms. Because most cases resolve within 3-6 months, doctors may monitor the condition before considering active treatment.
2. Laser Photocoagulation
Used to seal leaking retinal areas, particularly in cases where the leakage is persistent and pin-point. Only suitable for leaks that are located away from the fovea (the central part of the macula).
3. Photodynamic Therapy (PDT)
Involves injecting a light-sensitive dye (verteporfin) into the bloodstream, followed by laser activation to reduce choroidal hyperpermeability. Particularly effective in chronic and recurrent CSCR.
4. Anti-VEGF Injections
May be used in some cases to reduce choroidal vascular leakage. Drugs like Bevacizumab (Avastin) Ranibizumab (Lucentis) and Aflibercept (Eylea) may be considered.
5. Medications
Oral mineralocorticoid receptor antagonists (e.g., Eplerenone, Spironolactone) have shown potential in reducing fluid accumulation in chronic CSCR. Mifepristone, a glucocorticoid receptor antagonist, has been explored as a treatment. However, randomised controlled trial results did not support use of these medications.
Lifestyle Modifications for CSCR Management
Patients with CSCR can benefit from certain lifestyle adjustments to minimize the risk of recurrence and improve overall eye health.
1. Stress Reduction
• Practice relaxation techniques such as yoga, meditation, and deep breathing.
• Engage in leisure activities to reduce psychological stress.
• Consider counseling or cognitive behavioral therapy (CBT) if stress levels are high.
2. Avoid Corticosteroid Use
• If on steroids for another medical condition, discuss alternative treatments with your doctor.
3. Improve Sleep Hygiene
• Maintain a regular sleep schedule.
• Avoid excessive screen time before bedtime.
• Reduce caffeine intake, especially in the evening.
4. Dietary Changes
• Eat a diet rich in antioxidants (leafy greens, fruits, and nuts).
• Reduce salt intake, as excessive sodium can affect vascular health.
• Consider probiotics if H. pylori infection is suspected.
5. Limit Stimulants
• Reduce alcohol, nicotine, and excessive caffeine consumption.
6. Maintain Cardiovascular Health
• Control blood pressure and cholesterol levels through regular check-ups.
• Engage in moderate exercise such as walking or swimming.