Laser for Diabetic Retinopathy
Diabetic retinopathy is a common complication of diabetes mellitus that can have severe implications for vision. Treatment of advanced stage of diabetic retinopathy (also known as proliferative diabetic retinopathy) is with monthly anti-VEGF or retinal laser. Anti-VEGF treatment is repeated every month. Pan Retinal Photocoagulation (PRP) laser acts as permanent anti-VEGF.
What is diabetic retinopathy and how does it affect vision?
Diabetic retinopathy is a medical condition that occurs due to long-term, uncontrolled diabetes mellitus. Elevated blood sugar levels can cause damage to the small blood vessels in the retina, leading to leakage of blood and fluid into the retinal tissue. Initially, the condition is asymptomatic but can lead to progressive vision loss if left untreated. There are primarily two stages:
- Non-proliferative Diabetic Retinopathy (NPDR): Characterized by microaneurysms, hemorrhages, and mild retinal swelling.
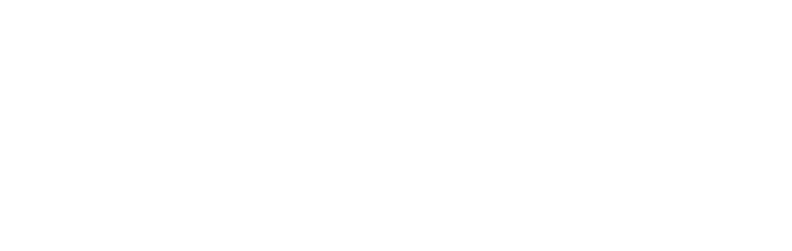
Diabetic Retinopathy- Mild Stage
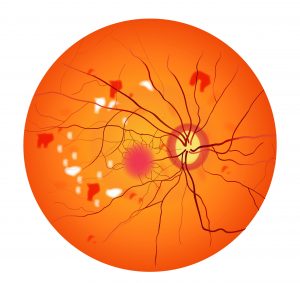
- Proliferative Diabetic Retinopathy (PDR): Marked by the growth of abnormal blood vessels on the surface of the retina, which can lead to severe vision complications, including retinal detachment and vitreous hemorrhage. Advance stages of PDR are also referred as Advanced Diabetic Eye Disease (ADED)

Diabetic Retinopathy- Advanced Stage
What is panretinal photocoagulation (PRP), and how does it work?
Panretinal photocoagulation is a laser treatment specifically designed to treat proliferative diabetic retinopathy. The laser energy is targeted towards the peripheral areas of the retina to induce controlled burns. This process shrinks abnormal blood vessels and helps to reduce the risk of severe vision loss. Essentially, PRP aims to reduce the metabolic demand of the peripheral retina so that the remaining blood supply can adequately sustain the central retina, which is responsible for sharp vision.

What are the indications for undergoing PRP?
The primary indication for PRP is proliferative diabetic retinopathy (PDR). Specific conditions where PRP is recommended include:
- Presence of Neovascularization: Growth of new, abnormal blood vessels on the retina or iris.
- Vitreous Hemorrhage: Bleeding into the clear gel that fills the eye’s center.
- High Risk Characteristics: Such as extensive blood vessel growth near the optic disk.
It is crucial to consult with a retina specialist for a thorough eye examination and appropriate diagnostic tests to determine if PRP laser is the right treatment option for you.
What does the PRP procedure entail?
The PRP procedure is usually carried out in an outpatient setting and typically takes about 5-10 minutes for the laser. The steps are as follows:
- Preparation: Your eyes will be dilated using eye drops. This process takes about 2 hours.
- Anesthesia: a topical anesthetic will be applied to numb the surface of the eye.
- Positioning: You will be seated comfortably in front of the laser machine.
- Treatment: A special lens will be placed on your eye to focus the laser beams accurately. The laser will deliver multiple burns in a scattered pattern on the peripheral retina.
- Post-Treatment: You will be observed for a short period before being discharged. If pain occurs later in the day, take tablet Panadol.
Each yellow dot represents a laser spot. Multiple laser spots are needed all around to treat the proliferative form of diabetic retinopathy (PDR).
What can I expect immediately post-PRP laser treatment?
After the procedure, you may experience some discomfort and blurring of vision, which usually resolves within a few hours to a couple of days. It’s essential to avoid driving immediately after the procedure.
Follow-up appointments are critical to monitor the healing process and assess the effectiveness of the treatment.
Are there any risks or complications associated with PRP?
While PRP is generally considered safe and effective, like any medical procedure, it comes with its set of risks and complications, such as:
- Reduced Peripheral Vision: As the laser targets the peripheral retina, there may be a reduction in your field of vision.
- Night Vision Issues: Difficulty in seeing in low-light conditions can occur.
- Light scattering
- Increased Intraocular Pressure: A temporary spike in eye pressure can occur post-procedure, which is usually well-controlled with medications.
Other Frequently Asked Questions
- Will PRP cure diabetic retinopathy?
– PRP is not a cure but a treatment to control the progression and mitigate the risks of severe vision loss.
- How many sessions will I need?
– The number of sessions depends on the severity of your condition and the response to treatment, often determined by your ophthalmologist.
- Is the procedure painful?
– Most patients experience minimal discomfort, managed effectively by topical anesthesia.
Disclaimer: This information is intended for educational purposes and should not be considered a substitute for professional medical advice.