Anti-VEGF injections
Anti-vascular endothelial growth factor (anti-VEGF) injections are therapeutic agents commonly used for treating specific eye diseases that cause vision impairment or blindness. This guide elucidates the indications, risks, procedure details, and alternative treatment options for patients considering anti-VEGF injections as part of their medical regimen.
What is Anti-VEGF?
Vascular Endothelial Growth Factor (VEGF) is a protein that promotes the formation of new blood vessels. While generally beneficial for wound healing and in the formation of the circulatory system, excessive VEGF production can be detrimental in certain ocular conditions. Anti-VEGF injections inhibit the action of VEGF, thereby curbing abnormal blood vessel growth and fluid leakage in the eye, which are often the underlying causes of vision loss in diseases such as age-related macular degeneration (AMD), diabetic retinopathy, and retinal vein occlusion.
Anti-VEGF injection
Indications for Anti-VEGF Therapy
1. Age-Related Macular Degeneration (AMD)
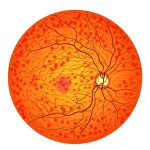
Wet AMD: Characterized by the abnormal growth of blood vessels in the macula, the central part of the retina. These vessels tend to leak fluid, leading to scarring and a rapid loss of central vision.
2. Diabetic Retinopathy
a. Proliferative diabetic retinopathy (PDR): Late-stage diabetic eye disease characterized by the growth of fragile blood vessels that can bleed into the vitreous, causing severe vision impairment.
b. Diabetic macular edema (DME): A complication of diabetic retinopathy, DME involves the swelling of the macula due to fluid accumulation.
3. Retinal Vein Occlusion: A blockage in the retinal vein leads to swelling and hemorrhages, causing vision loss. Anti-VEGF treatment may minimize swelling and improve vision.
Other Conditions:
Macular edema secondary to uveitis
Choroidal neovascularization not related to AMD
Rubeosis secondary to any cause
Procedure Details
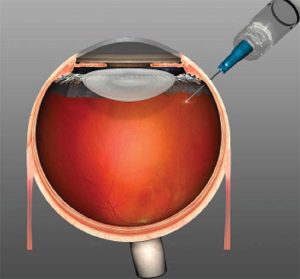
Local Anesthesia: Topical anesthetic drops are applied to numb the eye surface.
Sterilization: The eye and surrounding areas are disinfected with brown coloured povidone iodine.
Injection: A fine needle delivers the anti-VEGF medication into the vitreous, the gel-like substance in the eye’s center.
Post-procedure Care
Prescription of antibiotic drops to prevent infection
Follow-up visits for monitoring the eye’s response to treatment
Additional injections might be necessary, depending on the disease’s progression.
Complications
Irritation and watering: Hypersensitivity to the disinfecting medication might result in redness, itching, and irritation. This usually lasts for 24-48 hours maximum.
Subconjunctival Hemorrhage: Bleeding at the injection site can occur but typically resolves without treatment in 10-14 days.
Increased Intraocular Pressure: Temporary spikes in eye pressure are common but generally resolve within a day.
Retinal Detachment: Rarely mechanical injury from the injection could lead to a detachment of the retina.
Infection: Though very rare, endophthalmitis, an infection of the internal structures of the eye, can occur. This is a serious complication. Immediate medical attention is required. Significant drop in vision associated with severe pain is usually the initial presentation. Urgent medical treatment is required.
Alternative Treatment Options
For AMD
Photodynamic Therapy (PDT): A light-activated drug is used to seal off leaking blood vessels. Rarely used today because of scarring.
Laser Coagulation: High-energy light burns and seals the abnormal vessels but is rarely used today due to high risk of scarring.
For Diabetic Retinopathy
Panretinal Photocoagulation: Laser treatment to shrink abnormal blood vessels.
Vitrectomy: Surgical removal of the vitreous gel to clear blood and scar tissue.
For Retinal Vein Occlusion
Corticosteroid Implants: Steroids can reduce macular edema but come with a higher risk of complications like cataract formation and glaucoma.
Conclusion
Anti-VEGF injections are a pivotal treatment option for several vision-threatening diseases. However, the procedure comes with its set of risks and complications that require a comprehensive discussion with your healthcare provider. Multiple treatment sessions may be necessary for optimal outcomes. Alternative therapies do exist but are generally considered less effective or riskier.
For personalized advice, consult your ophthalmologist to discuss the most suitable treatment options for your condition.
Disclaimer: This information is not a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition.